Interventions
Career surgeons and medical professionals are exposed to specific job-related ergonomic challenges that can contribute to musculoskeletal disorders (MSDs), burnout and early retirement. Dr. Hallbeck's Human Factors Engineering Lab team works to discover and mitigate the root causes of these issues using a variety of interventions.
Exoskeletons
Health care workers are commonly exposed to postures that present a high degree of ergonomic risk to practitioners. For example, cardiac ultrasonographers who perform transthoracic echocardiograms (TTEs) have a particularly high risk of developing injuries of the arm and shoulder due to the nature of their work. These injuries involve abducted shoulders, coupled with static exertions to obtain good-quality images. This study examined the effectiveness and usability of two separate models of arm-support exoskeletons to reduce fatigue and muscle activity while scanning. Postures and subjective body-part discomfort also were collected. Electromyograms (EMGs) were used to measure muscle activity in the arms and upper body, while inertial measurement units (IMUs) were used to measure postures.
Dr. Hallbeck also is working with surgeons to assess intraoperative exoskeletons. Her team is testing both back and neck support passive exoskeletons to determine if they reduce pain and fatigue in long, complex surgeries to improve surgeon wellness. The lab has introduced and tested back-support exoskeletons with surgeons in the operating room to determine their usability and acceptability in the OR environment.

A surgeon wears a loupe while operating.
Loupes
Surgeons are susceptible to developing MSDs due to their exposure to high-risk postures held statically during operations. The neck is an area of exceptionally high risk to surgeons due in part to extended periods of neck flexion while performing surgery. Additionally, the use of loupes has been shown to be a contributing factor to these high-risk postures that may lead to disorders of the cervical spine. Prismatic loupes present a potential solution to this issue, as their use allows the surgeon to view the surgical field without needing to flex their neck, potentially improving their neck posture and risk of musculoskeletal disorders. The lab's team plans on using IMUs to study the differences in postures between surgeons who use traditional loupes versus those who use prismatic loupes, to determine whether loupes are a viable intervention.
Exoscopes
Plastic surgery has been shown to present a high degree of ergonomic risk for surgeons. A common procedure performed is the deep inferior epigastric perforator (DIEP) flap surgery. DIEP flaps are of particular ergonomic importance as the procedure involves using multiple surgical techniques and equipment. These include open surgery with loupes and microsurgery using a surgical microscope, high-risk postures, and an average operating duration of more than 10 hours.
The exoscope consists of a camera mounted on a semi-robotic arm manipulated by the surgeon to image the surgical field. The view of the surgical field is then displayed on a monitor in either 4K or 3D. In this study, Dr. Hallbeck's group compared exoscope use with traditional equipment consisting of loupes, headlights and microscopes to perform the DIEP flap procedure.
The goal of this project was to evaluate the effectiveness of the exoscope in normalizing intraoperative postures, thereby reducing the ergonomic risk associated with the DIEP flap procedure when compared to using traditional equipment, such as loupes, headlights and microscopes.
Compared with the traditional equipment, the exoscope was able to normalize postures and, as a result, decrease the ergonomic risk associated with performing DIEP flap surgery without substantially increasing surgical duration. In this study, the lab's team concluded that the exoscope was able to normalize postures during the DIEP flap surgery when used as an alternative to traditional loupes, headlights and surgical microscopes.
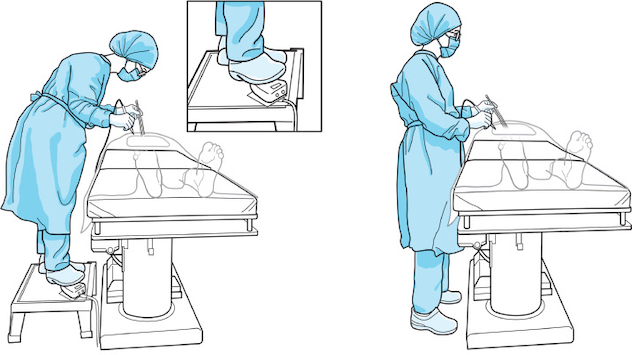
An illustration of improper ergonomic postures (left) versus proper postures (right) during open surgery.
Education
Despite the presence of ergonomic risks associated with performing surgery, there is still a lack of surgical ergonomics education in residency programs. This often results in a lack of awareness of ergonomics among surgeons throughout their careers, which may lead to poor postures and contribute to the development of work-related musculoskeletal disorders. These injuries negatively impact surgeons' well-being and may result in shortened careers and early retirements due to these occupational injuries sustained because of performing surgery.
Using the available literature on surgical ergonomics, the lab has created a set of educational modules on proper postures and equipment setup during surgery. Aimed at both residents and attending surgeons, these modules are designed to educate surgeons on the importance of surgical ergonomics and proper ergonomic practices. After completing the course, residents will be able to identify and correct high-risk postures when operating, proper ergonomic operating room setups and the importance of good ergonomics throughout their careers. Recent evaluation of this module is published in the surgical education literature.
OR Blackbox
The operating room is a complex and safety-critical working environment. It is difficult to study, due in part to sterility and privacy concerns. Nevertheless, it is important to study OR operations to improve teamwork and patient care outcomes. To accomplish this, Mayo Clinic has installed the OR Black Box (ORBB), an AI-enabled system, in some ORs. The ORBB is a device that uses cameras and microphones to collect, de-identify audiovisual (AV) data, and then analyze the data collected during surgery to reduce medical errors and improve patient safety and OR efficiency. Introducing an AI-enabled AV device into the operative environment was done with care as the team worked to ensure patient and provider anonymity and psychological safety. The ORBB has allowed surgical teams to enhance surgical morbidity and mortality reviews. "Aggregate data is deidentified and anonymized so that we can learn from it now and in the future, and audiovisual data is deleted after 30 days to protect the privacy and confidentiality of patients and healthcare providers," Surgical Safety Technologies founder Teodor Grantcharov, M.D., Ph.D., a professor of surgery and practicing surgeon at Stanford Medicine, said in this article.
Bringing in ORBB has resulted in "a lot of positive changes around teamwork and team function and how we respond to things," Sean P. Cleary, M.D., a surgical oncologist at Mayo Clinic, said. "When we have something happen in the operating room and the team's able to respond to a change in plan and done so smoothly and efficiently, we can now characterize that."
Whereas "traditionally, it was a bunch of surgeons and nurses in a room together retrospectively recollecting what happened, and to say it was subjective would be very kind," Dr. Cleary said. "What this has done is allowed us to bring some objective data into that discussion."
The human factors team is currently investigating the use of the ORBB to improve patient safety and outcomes, OR efficiency, and OR staff safety and productivity.